RPM Overview
By: Robert Longyear
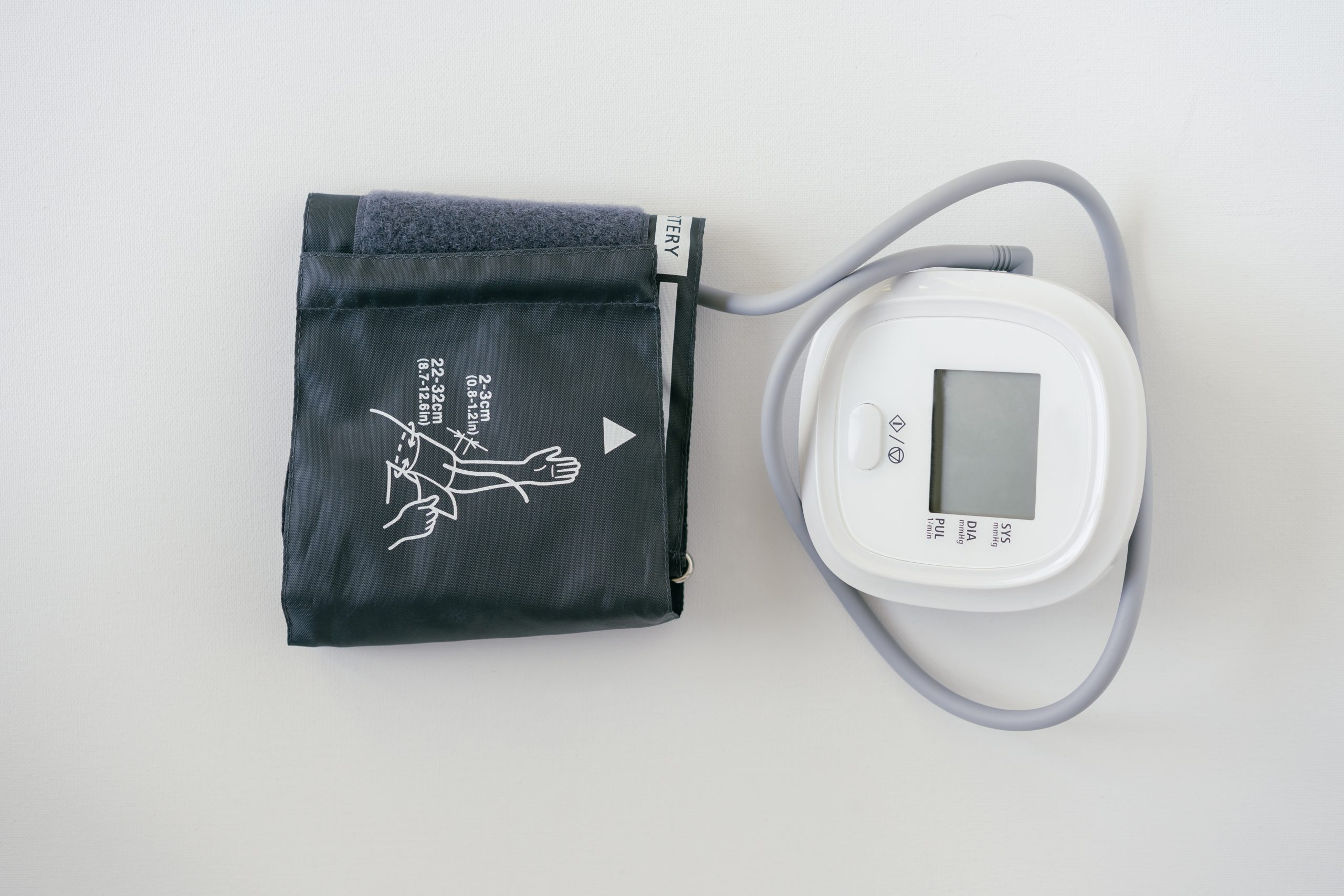
Remote patient monitoring (RPM), or remote-physiological monitoring, is a model of care that involves the collection and transmission of clinical data from patients to a healthcare provider. RPM is a topic of significant interest due to its clinical effectiveness and potential to generate savings. The model of care enables a more proactive approach to both chronic and acute conditions. Typically, a patient receives a medical device that will be relevant to the patient’s condition e.g. a blood pressure cuff for hypertension or a blood glucometer for diabetes. This device will connect to either a mobile application via a smartphone with Bluetooth capabilities or will transmit the data via cellular networks (e.g., 4G, 5G). The healthcare provider is on the receiving end of the RPM technology and can then view patient data in real-time rather than waiting to collect a single point of data each three months as is common in chronic disease care.
Once a healthcare provider has patient data flowing in through an RPM platform, the information can be used to glean important information about the performance of the patient’s care plan, can alert providers to immediate clinical needs, and can incentivize patients to be more active in managing their own healthcare needs. It is important to note that while “monitoring” is in the name, the program has tangible and well-documented benefits for patient education and self-care behaviors.
Medicare rolled out reimbursement for RPM services in 2018/2019 and the model has gained a good deal of attention from tech companies, healthcare providers, policy makers, and Wall-street. Rightly so, as the outcomes that are observed from RPM can generate significant economic savings for the health system as a whole and for patients who may avoid an unnecessary emergency department visit or who may benefit from the effective long-term care services for chronic disease that RPM affords.
For example, a patient with hypertension may have been prescribed a new medication at their last clinic visit. Typically, the patient may return to the clinic for a check-up three months from the most recent visit. However, with RPM, should the patient’s blood pressure continue to rise despite medication, the care team is able to step in before the patient ends up in the hospital.
During Covid-19, RPM became a model of care that was increasingly viewed as a remedy for the infection risks associated with in-person care at a brick-and-mortar clinic visit. Thus, it is expected that claims would increase from 2019 to 2020.
|
CPT Code |
CPT Code Descriptor |
National Average Reimbursement |
|
99453 |
Initial Set-Up; Patient Education |
$21 |
|
99454 |
Device cost, data transmission each 30 days |
$69 |
|
99457 |
20 minutes data review; clinician time; interactive communication |
$54 |
|
99458 |
20 minutes data review; clinician time; interactive communication |
$43 |
|
99091 |
30 minutes data review; QHP time; interactive communication |
$56 |
Definitiv Healthcare RPM Claims Data Volume
Definitiv Healthcare, a healthcare data company, has reported the following data from 2019 and 2020. These are not the full code-sets for RPM, but the overall trend is important to note.
|
CPT Code |
Description |
2019 Claims Volume |
2020 Claims Volume |
% Change |
|
99453 |
Patient Set-Up (15 Minutes) |
13,183 |
61,159 |
363.9 |
|
99454 |
RPM Data Transmission (16 Days) |
36,200 |
229,133 |
533 |
|
99457 |
20 minutes clinical staff time |
32,551 |
184,149 |
465.7 |
|
99458 |
30 minutes of time by QHP |
72,441 |
69,883 |
-3.5 |
Fig. 1 Data from Definitive Healthcare’s ClaimsMx product for calendar year 2019 and 2020. Commercial claims data is sourced from multiple medical claims clearinghouses in the United States. Data is updated monthly—accessed May 2021.
The only CPT Code with a slight decrease in volume was CPT 99091. It is important to note that during this period, CMS introduced CPT codes 99457 and 99458 which allow clinical staff as opposed to the physician to manage the clinical time component of an RPM program. This is likely why the decrease occurred and will likely continue.
This data provided by Definitiv is one of the few quantitative reviews of RPM claims data with respect to volume and utilization. Assuming patients participate in the program for 3 months on average with the services billable each month, the number of patients that have received RPM data transmission in 2020 would be approximately 76,000 patients. To put this in perspective, there were 62.6 million Medicare beneficiaries in 2020.
Remote-patient Monitoring Growth
According to some estimates, the global RPM market size was $25.48 Billion in 2020 and is expected to grow to between $48 M and $115M by 2026. Regardless of exact market size, the level of venture investment in the digital health space has reached greater than $14 B in 2020. Clinically speaking, RPM has a strong evidence-base in the academic literature. A review of PubMed quickly reveals that RPM has been studied extensively over the past decade. The U.S. Agency for Healthcare Research and Quality has recommended RPM be implemented clinically and has called for more concrete research into implementation factors that lead to successful programs as the clinical value has been established. At Longyear Health, we expect the RPM market to accelerate rapidly.